CE / CME
Obesity Management During Women’s Reproductive Years: Expert Insights to Your Clinical Queries
Physician Assistants/Physician Associates: 1.00 AAPA Category 1 CME credit
Nurse Practitioners/Nurses: 1.00 Nursing contact hour
Physicians: maximum of 1.00 AMA PRA Category 1 Credit™
Released: October 29, 2025
Expiration: October 28, 2026
Activity
Patient Case 1: Susan, 30-Yr-Old Woman, G0P0
Susan is a 30-year-old woman who has a BMI of 32 kg/m2. She was diagnosed with PCOS as a teenager and has very irregular menstrual cycles and insulin resistance (A1C 5.6%). Susan has been trying to conceive for 6 months. She has ongoing concerns about her fertility and weight gain; she has gained 10 lb in the past year. Susan is understandably frustrated. She walks 3-4 times a week and is cutting back on carbohydrates.
This is a patient who we all see every day. Susan is motivated, but she is struggling against the hormonal and metabolic challenges of PCOS.
Patient Case 1 Discussion
Susan's goals are to regulate her cycles and conceive. Since modest weight loss of 5% to 10% can improve her fertility, it would be good to have conversations with her about weight loss, cycle regulation, and fertility. Because she is trying to conceive, discussion of safe, supportive therapies is also important.
PCOS biology, specifically insulin resistance and increased androgen levels, can also be a barrier to reaching her goals. Then we can think about her emotional stress and stigma, including how that might affect her weight and health. It certainly takes a lot of courage for patients to walk into the exam room and have these conversations with us.
Medication options are limited for patients who are trying to conceive, and there are challenges with accessing agents that are approved. Therefore, focus on lifestyle modifications—specifically nutrition, physical activity, and sleep—might be a good direction for Susan. So how can these tools be used to help Susan reach her goals?
One thing to talk about with patients is physical activity intensity—how much they need to raise their heart rate. That does not mean that they have to go for a jog or run. Wearables are good tools for monitoring activity intensity, but patients do not always have access to those. Identifying a target heart rate can help patients understand how to push themselves, or the target can be simplified by telling the patient they should push themselves enough that they have trouble singing but can still talk during the activity.
A key component of Susan’s care is her PCOS; the insulin resistance and androgens are important barriers she is facing. Focusing on nutrition, physical activity, and sleep can help Susan achieve her health goals. Adding metformin is also a consideration, for insulin sensitivity and cycle regulation, and incretin-based therapy may also be an option. If it is acceptable to Susan to delay conception efforts, she could use an incretin-based therapy and discontinue it before trying to conceive. The takeaway message is that advising realistic goals of 5% to 10% weight loss can help patients like Susan achieve ovulation restoration.
Impact of Obesity and PCOS on Fertility
This diagram explains Susan’s case; this is her biology. PCOS and obesity overlap to worsen insulin resistance and inflammation, which drives increased androgen levels. These elevated androgens disrupt ovulation and impair both oocyte quality and endometrial receptivity.34 The end result is subfertility, and OB/GYN HCPs see patients like this every day.
The best thing that OB/GYN HCPs can do is reassure patients that this is their biology and the pathophysiology of PCOS and obesity. It is not their fault. Tell patients that you are partnering with them, you see them, and this is not their fault. In a nutshell, modest weight loss can improve ovulation and fertility outcomes, medications like incretin-based therapies may reduce insulin resistance and androgen levels, and shared decision-making is critical.
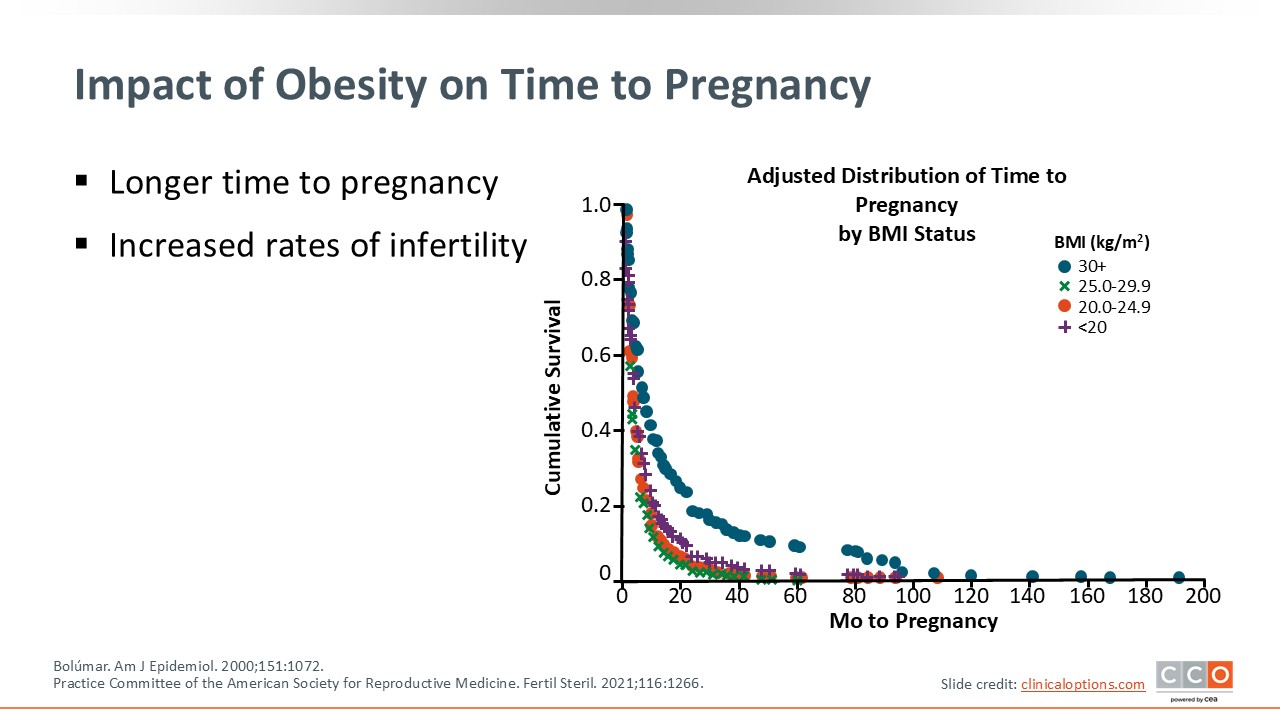
Impact of Obesity on Time to Pregnancy
Women with higher BMIs take significantly longer to conceive. This figure shows what this effect looks like at the population level. Infertility rates also increase with BMI.32 For Susan, this helps frame why addressing weight and metabolic health can be important for improving her fertility outcomes.
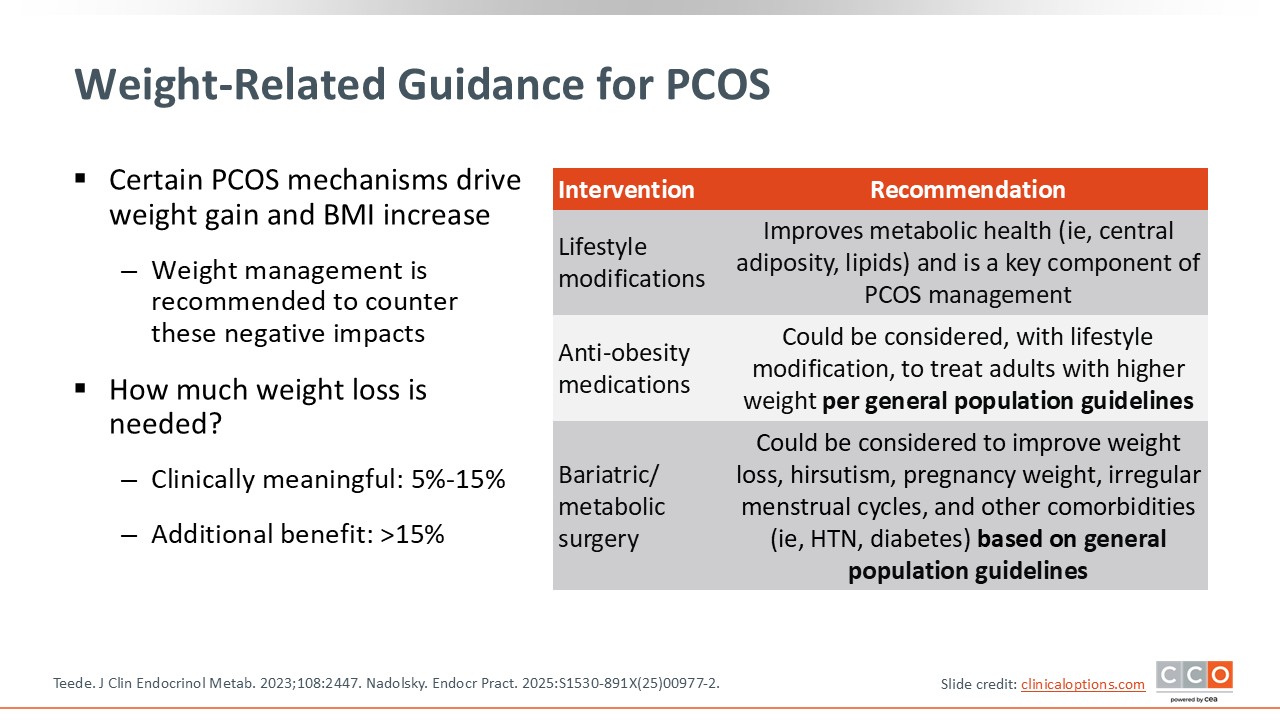
Weight-Related Guidance for PCOS
How much weight loss is meaningful? Even a modest reduction of 5% to 15% can restore ovulation and improve menstruation cycles. Weight loss beyond 15% will add additional metabolic and fertility benefits. For Susan, 5% to 10% weight loss would be realistic and clinically meaningful.
However, it is important to note that PCOS is driven by mechanisms that make it harder for patients to lose weight: insulin resistance, androgen excess, and metabolic dysfunction. This is why obesity care is central to PCOS management. You cannot address one without the other. Current guidelines recommend lifestyle modifications as first-line treatment. This includes diet quality, increased physical activity, sleep improvement, and monitoring lipids and metabolic health. These pieces are going to be the mainstay of PCOS and obesity management.
AOMs can be added when lifestyle modifications alone are not enough. Use of incretin-based therapies can promote weight loss and improve insulin resistance, which will directly address PCOS biology. Metabolic/bariatric surgery may be appropriate for select patients, but it is important to remember the time frame for delaying pregnancy after surgery.
Recognizing that there are situations where a patient can have PCOS without overweight/obesity, the key takeaway is that, in patients who have PCOS with overweight or obesity, weight management is not optional. It is therapeutic. If OB/GYN HCPs are managing patients with PCOS and overweight or obesity, whether they are concerned about fertility or not, they must discuss weight management.5,35
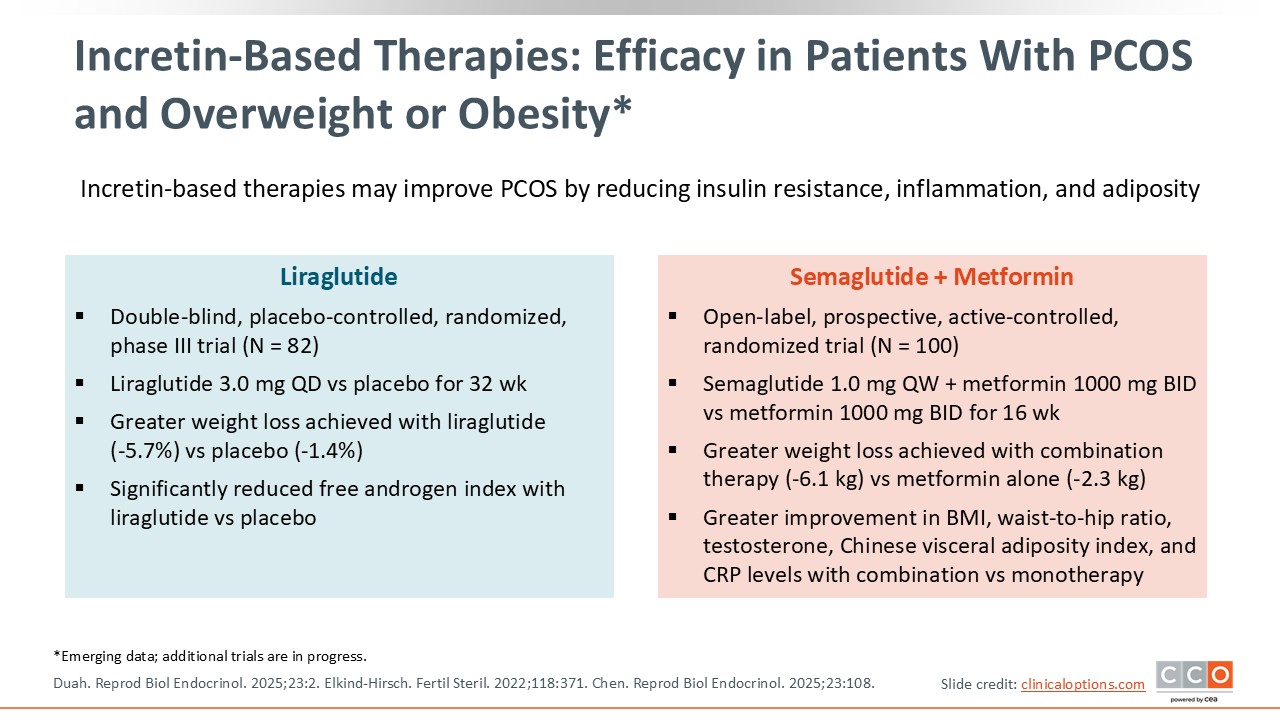
Incretin-Based Therapies: Efficacy in Patients With PCOS and Overweight or Obesity
There are emerging data on the use of incretin-based therapy for patients with PCOS and overweight or obesity. These data are promising, as they show greater weight loss and reduced androgen levels compared with placebo. Of note, semaglutide plus metformin outperformed metformin alone. Hormonal improvements were also seen with this treatment.36-38 These therapies may help patients like Susan address both obesity and PCOS physiology together. However, it is important to be careful regarding the timing of incretin-based therapy treatment and attempted conception.
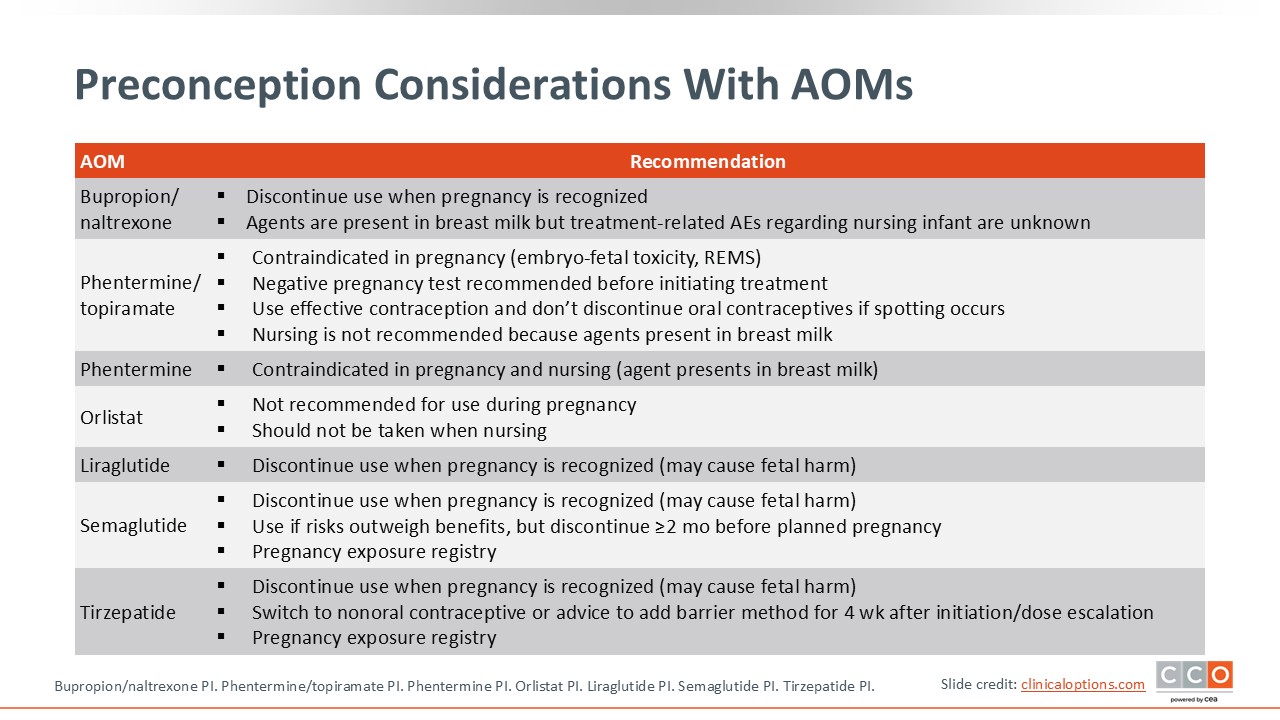
Preconception Considerations With AOMs
As a rule, OB/GYN HCPs should not recommend weight loss during pregnancy. Therefore, AOMs are not indicated for weight loss during pregnancy and should be stopped once a pregnancy is recognized.
However, there are patients who are receiving medications that are sometimes used to help with weight loss when they become pregnant—agents like bupropion, naltrexone, stimulants, or metformin—but this does not necessarily mean that those medications should automatically be stopped. For example, patients may be receiving metformin or naltrexone as part of their in vitro fertilization protocol, or even for other reasons. It is important for OB/GYN HCPs to dig in and understand why each medication is being used and whether it can and/or should be continued through the pregnancy. That is why we, as OB/GYN HCPs, must work with our psychiatry, addiction medicine, and reproductive endocrinology colleagues closely.
Two types of medication, topiramate and incretin-based therapies, deserve special consideration. Topiramate poses clear teratogenic risk to the fetus, including cleft lip and/or palate.39 Preconception counseling is critical for patients receiving topiramate, and although they should discontinue topiramate if trying to conceive, it is not always as simple as just stopping the medication. For example, a patient receiving topiramate for migraines who wants to conceive should continue topiramate and birth control until she has conferred with her neurologist and there is a medication plan that is adjusted based on her desire to become pregnant. The situation would be the same for patients who are receiving this medication for overweight or obesity.
The incretin-based therapies liraglutide, semaglutide, and tirzepatide have not been identified to have teratogenic effects in humans. Although there are animal data that suggest these agents may have teratogenic effects, data from registries of women exposed to these agents during pregnancy are reassuring. However, more evidence in humans is needed. So at this time, discontinuation of these therapies is recommended when pregnancy is recognized because there may be risks to the fetus and weight loss during pregnancy is generally not encouraged.26-28
A big challenge when stopping incretin-based therapies before conception is rapid weight regain.40 Patients may go through the necessary preconception counseling, start the medication to optimize health for pregnancy, and achieve good weight loss. However, when they stop taking the medication for a washout period, in some cases 2 or more months, they start to regain weight before they become pregnant, so they may contact you—their OB/GYN HCP—to ask if there is a way to change their plan and do something different.
This provides an opportunity for OB/GYN HCPs to work with patients and figure out a personalized approach. What is the patient’s nutrition plan? What is their activity level? What is their sleep quality? What are their stress levels? Can these factors be addressed to help support the weight loss they have achieved? Maybe it’s possible to transition them to another medication, like metformin. When an AOM is stopped as part of the patient’s plan, it is important to avoid undoing the benefits the AOM provided, and rapid weight regain can increase risk of gestational diabetes and preeclampsia. This scenario illustrates why preconception counseling is critical.