CE / CME
Obesity Management During Women’s Reproductive Years: Expert Insights to Your Clinical Queries
Physician Assistants/Physician Associates: 1.00 AAPA Category 1 CME credit
Nurse Practitioners/Nurses: 1.00 Nursing contact hour
Physicians: maximum of 1.00 AMA PRA Category 1 Credit™
Released: October 29, 2025
Expiration: October 28, 2026
Activity
Obesity: Highly Prevalent, Chronic Disease
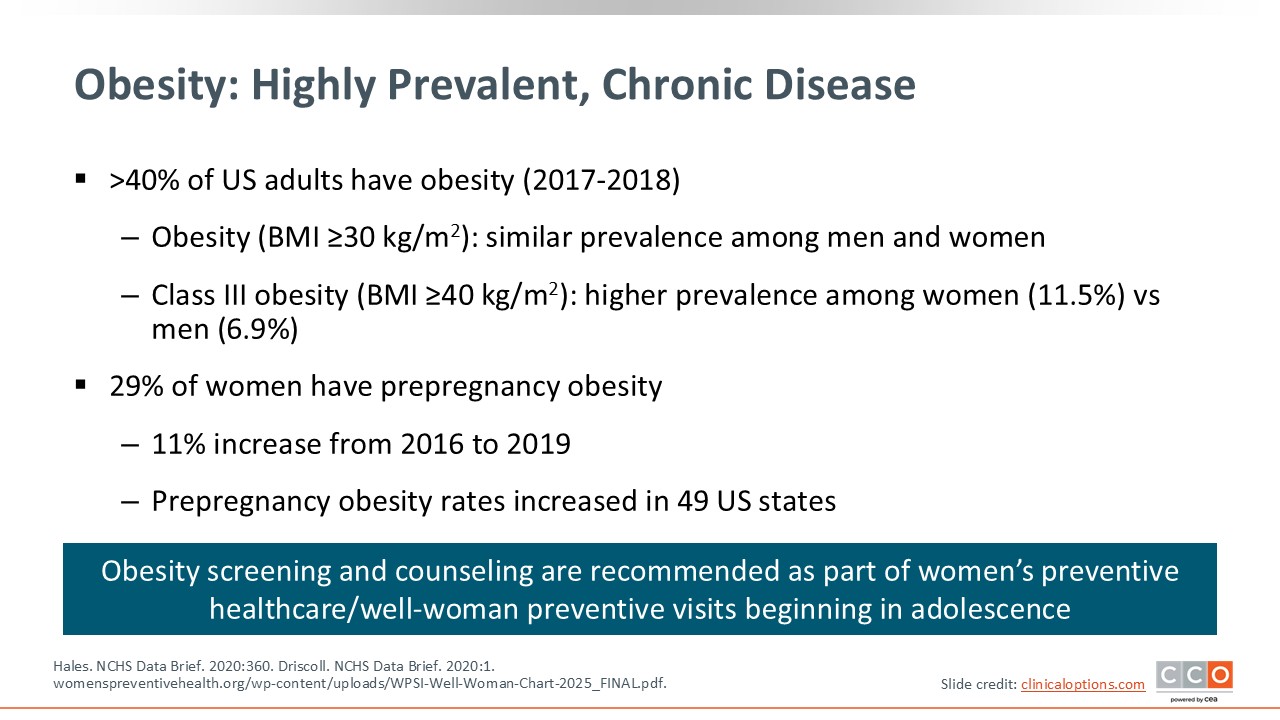
Obesity is a chronic disease. It affects more than 40% of US adults.1 It is also important to note that nearly 1 in 3 women will enter pregnancy with obesity, and that rate is rising across the US.2 This makes obesity management a core focus of women's health, not just a primary care and endocrinology issue. This is something that OB/GYN HCPs are seeing every day. In the clinic, on the labor floor, in high-risk pregnancy cases, and in postpartum care, we are seeing the effects of obesity on women’s health every day.
Significant and Complex Impact on Reproductive Health
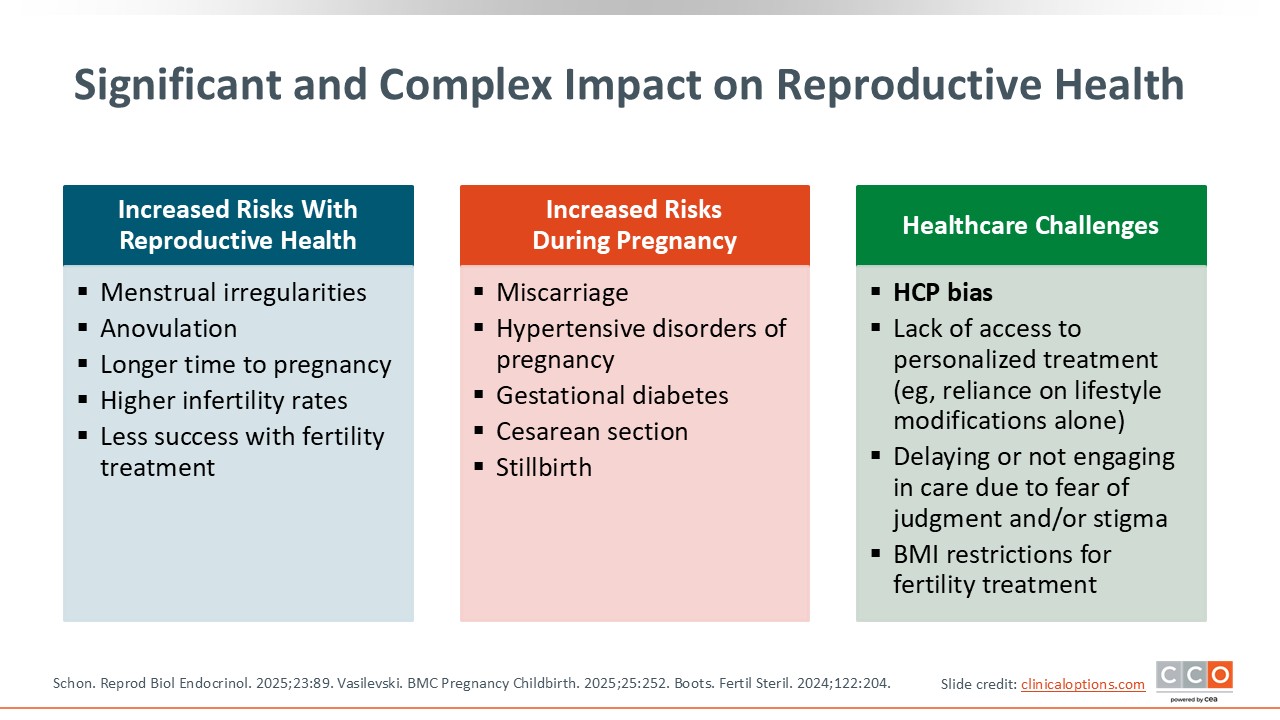
We know that obesity has a significant impact on patients’ reproductive health. Among those with obesity, risk of infertility is 3 times higher and it takes much longer for them to conceive vs those without obesity.3 Modest weight loss (5%-10% or 15%) can significantly improve ovulation rates in conditions like PCOS.4,5 Furthermore, obesity before and during pregnancy increases patients’ risk for multiple undesirable outcomes, including gestational diabetes, hypertensive disorders, and cesarean section.6,7
For the fetus and newborn, the risks associated with maternal obesity extend to increased risk of stillbirths, congenital anomalies, macrosomia, and neonatal intensive care unit admissions.7-9
OB/GYN HCPs have the benefit of seeing patients through their 9 months of pregnancy and beyond. I am the primary care provider for many of my patients. This is important because women often retain excess weight postpartum, leading to increased long-term risk for type 2 diabetes (T2D) and cardiovascular disease.10,11 OB/GYN HCPs may be the only healthcare touchpoint for women for many years, so we must be available and able to do the all-encompassing work that is needed. We have the unique opportunity to counsel, support, and guide patients with evidence-based strategies—not just for pregnancy-related outcomes but also for long-term maternal and child health.
Importantly, all HCPs should be aware of bias, whether within the healthcare system or individual HCPs, including ourselves. This is an entire topic all on its own. It is a big challenge in the healthcare system, including OB/GYN practice, and it is crucial that it is addressed.12
Diagnosing and Classifying Obesity
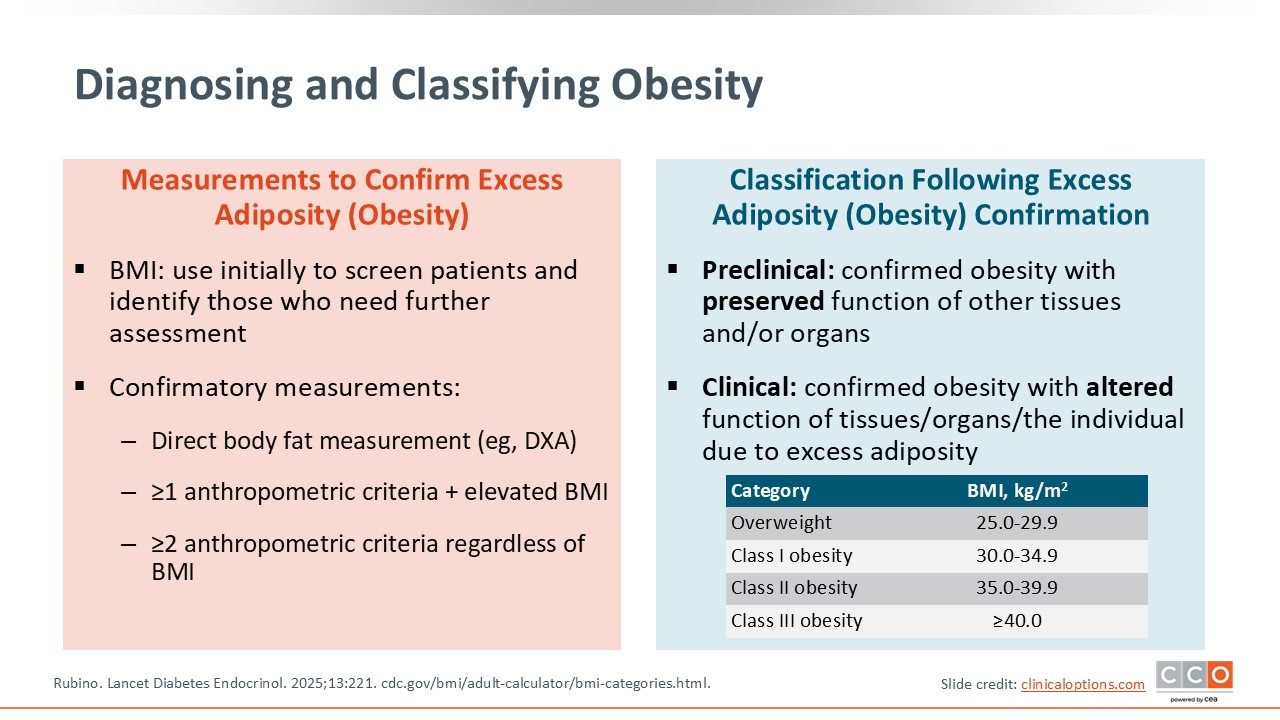
So how do we diagnose and classify obesity? HCPs are likely to be very familiar with BMI; that is the starting point. Obesity is classified by BMI: class I obesity is 30.0-34.9 kg/m2, class II obesity is 35.0-39.9 kg/m2, and class III obesity is 40.0 kg/m2 and above.13 Note that we have moved to using newer diagnostic codes, which refer to these obesity classes, and away from older “E66” codes, which describe obesity using terms like “morbid (severe) obesity due to excess calories”. This is at least in part because the words used for the older codes are associated with blame and shame. Codes for the revised, newer classifications are now available for use in electronic health records (EHRs).
Health risks increase with BMI level, but that is only part of the story. BMI does not tell it all. There are other staging systems that add depth to understanding patients’ health and well-being. For example, the Edmonton Obesity Staging System looks at the medical, functional, and physiological impact of obesity, not just BMI.14 More specifically, for OB/GYN HCPs, the Kings Obesity Staging Criteria adds reproductive and psychosocial domains to identify issues like PCOS, infertility, pregnancy complications, and stigma.15 These are helpful tools, and OB/GYN HCPs should ensure that they are familiar with them.
These tools do a better job of classifying and staging obesity vs using BMI alone. It takes patient care a step further by acknowledging that it is not just the number on the scale. BMI indicates how “big” a patient is, but staging tells us how sick and impacted they are. When used together, BMI and staging tools provide a more accurate and respectful framework for care.
Obesity assessment can be further nuanced with other measurements, including anthropometric measurements like waist circumference. We all have tape measures in our clinic for measuring fundal height, and they can also be used to confirm patients’ waist circumference. This does not need to be done with every patient all the time, but it is going to provide more information when needed.
Measurements of body composition using DEXA scan or impedance measurement provide additional pieces of information on the percentages of a patient’s body weight that are due to water, fat, and muscle mass. But these tools are expensive and not necessarily accessible at every clinic. Rather, it is something to be aware of as potential options.
Finally, we are fond of running labs in healthcare, and many of us are doing so to get additional pieces of information on patients’ health. Maybe that is to understand their glycated hemoglobin (A1C), lipids, liver enzymes, and/or thyroid-stimulating hormone. All these things are incredibly relevant when thinking about reproductive-aged OB/GYN patients with obesity. Insulin and androgens can also be added if PCOS is suspected. The key here is shifting from a number on the scale to the real health impact of obesity—meaning HCPs are providing individualized, patient-centered care.16
Obesity Treatment Pyramid: Weight Loss Potentially Achievable With Different Interventions
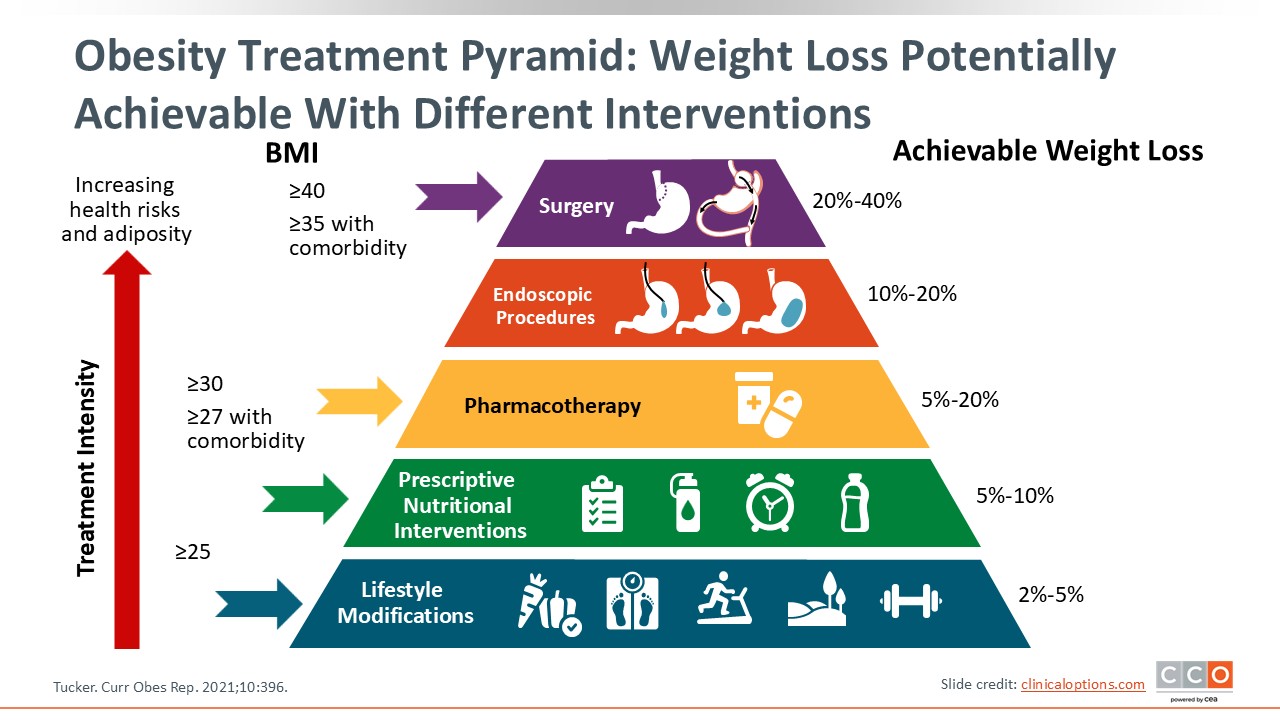
This slide shows a treatment pyramid for managing patients with overweight or obesity.17 Lifestyle modifications (ie, nutrition, physical activity, sleep, behavioral support) make up the base of the pyramid. These are the cornerstones for all patient care. This also is where HCPs need to partner with nutritionists, dietitians, diabetes educators, and physical therapists, among others, to provide multidisciplinary care.
Next, the pyramid moves into the more structured nutritional strategies, with meal planning, fasting protocols, hydration, and intensive tools. Again, dietitians, nutritionists, and diabetes educators can help with this level of care.
Moving into pharmacotherapy, this is an approach that is now central to comprehensive obesity management and that many OB/GYN HCPs are providing. Available pharmacotherapies can help patients achieve as much as 15% to 20% weight loss. In the SURMOUNT-5 trial comparing tirzepatide and semaglutide, ≥25% weight loss was achieved by 32% and 16% of patients receiving tirzepatide or semaglutide, respectively.18 Yet some of the AOMs are not new. We have been using pharmacotherapy in slightly different ways to help patients lose weight, but newer incretin-based therapies are making the significant differences in weight loss—comparable to weight loss with metabolic/bariatric surgery—that we are seeing today. Notably, pharmacotherapy can be a very useful tool in obesity management, but it is important to document a contraception plan for all patients with pregnancy potential.
Endoscopic and surgical options are at the top of the pyramid and include sleeve gastroplasty and balloons that help patients achieve 10% to 20% weight loss, depending on the procedure. Metabolic/bariatric surgery delivers the most effective and durable results of 20% to 40% weight loss. These are procedural approaches performed by bariatric teams; OB/GYNs HCPs coordinate referral and timing. We can help patients with lifestyle modifications and prescribing AOMs, but we must refer to our bariatric colleagues for patients interested in surgery. It is also important to note that these approaches require careful timing in reproductive-age patients.
The key point is that obesity management does not have to follow a rigid ladder. HCPs can tailor care based on needed intensity and patients’ goals, risks, comorbidities, and reproductive plans. Where patients are with goals, health, etc will inform what part of the pyramid is most relevant, and this brings back the need for individualized and respective care in the management of overweight or obesity.17
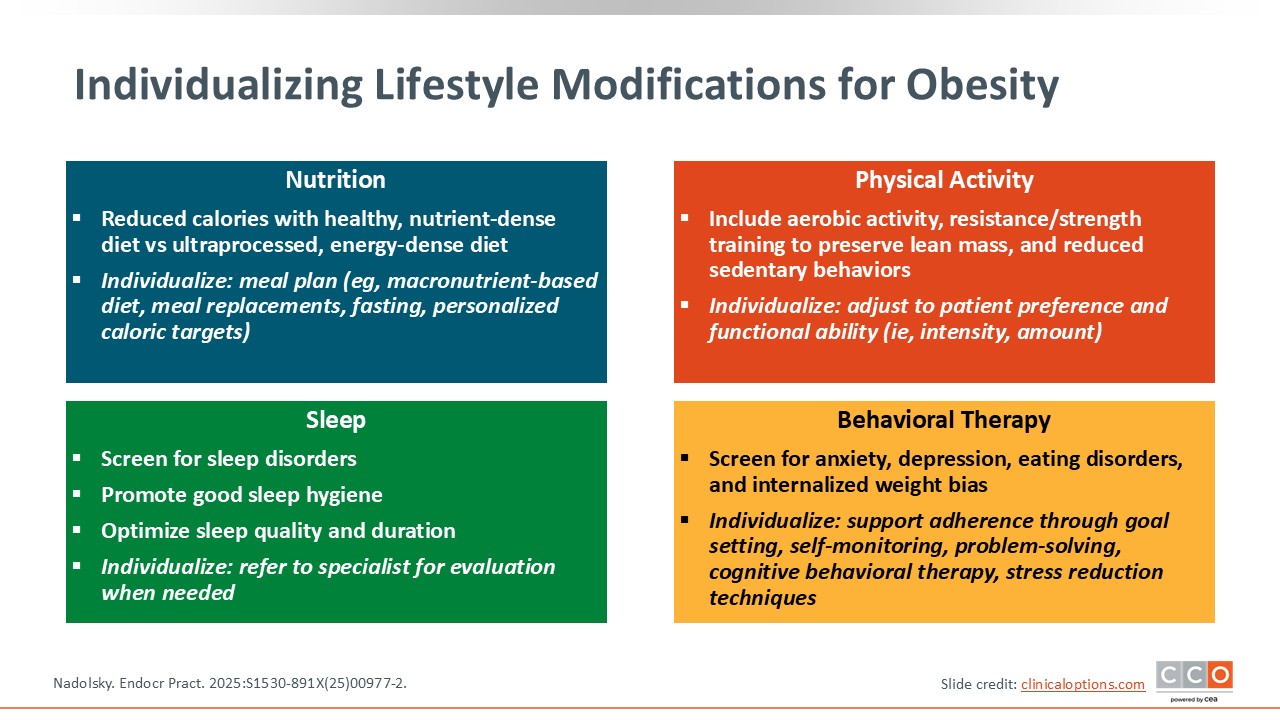
Individualizing Lifestyle Modifications for Obesity
Managing patients with overweight or obesity builds on the foundation of lifestyle modifications. Even when prescribing AOMs, HCPs should be counseling patients about their nutrition, physical activity, sleep, and stress levels. Treatment goes better when AOMs are used with lifestyle modification, and there is a much better relationship with patients when we provide comprehensive care. OB/GYN HCPs in the women's health space generally do well at partnering with patients, and lifestyle modifications are a part of that.
Patients should have realistic meal plans and participate in physical activity that is matched to their abilities. If a patient is in a wheelchair, it is not realistic for them to train for a 5K running race. Instead, focus should be on identifying a physical therapy activity plan that can keep them safe and free from injury. We need to address mental health and weight bias, and sleep is also critical. The Epworth Sleepiness Scale or STOP-BANG can be used to screen for sleep issues like obstructive sleep apnea.19-21
To provide patients with access to as many obesity management interventions as possible, including AOMs, HCPs need to know what other comorbidities patients have, and sleep apnea is huge during pregnancy. HCPs should know what a patient’s risk is so they can have their continuous positive airway pressure machine with them when in labor if needed.
OB/GYN HCPs need to look at all of these different pieces through the lens of women’s health as well as obesity medicine. Lifestyle modifications, again, remain central no matter what additional treatments are used. They anchor every step.5
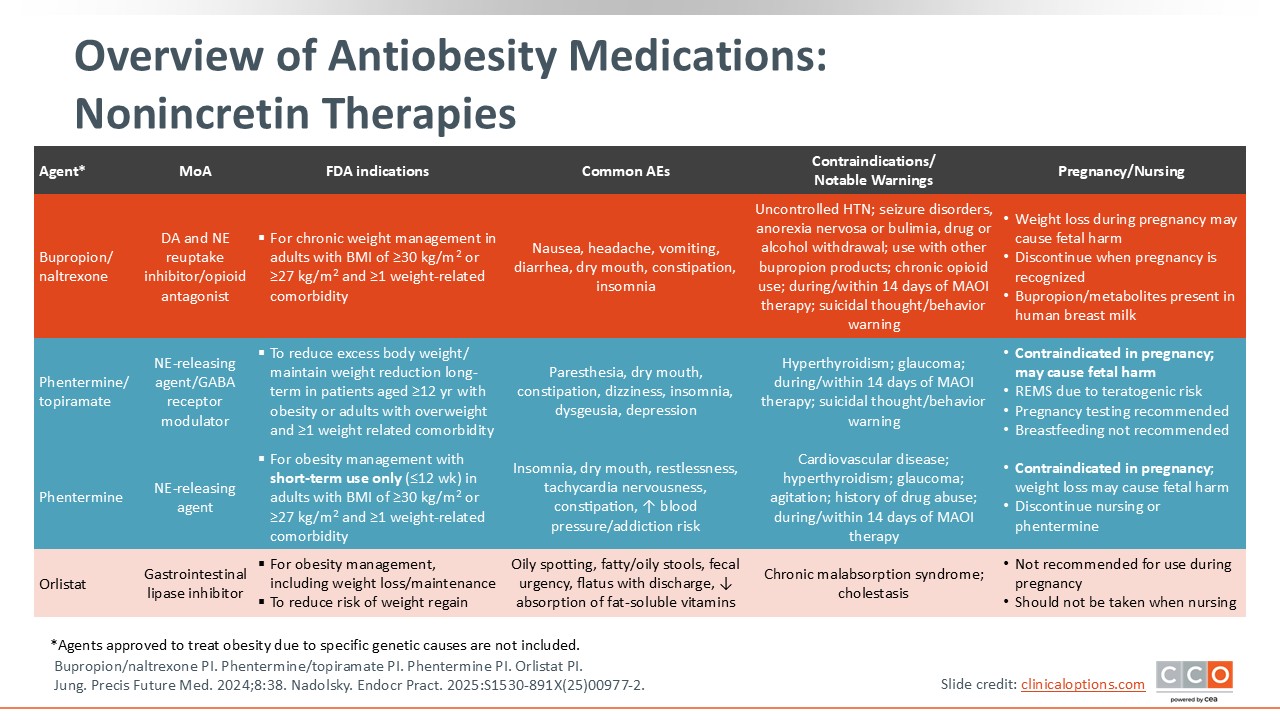
Overview of Antiobesity Medications: Nonincretin Therapies
The accompanying slide provides a lot of information on AOMs. The therapies on this slide are not new. Medications for obesity management have been available for a long time, but they have not demonstrated the same successes as newer incretin-based therapies.
Phentermine, phentermine/topiramate, orlistat, and bupropion/naltrexone work through different mechanisms and carry unique safety profiles.22-25 The key is matching the right agent to the right patient based on their comorbidities, reproductive goals, and preferences.
It is worth noting that just because some of these AOMs combine medications, HCPs do not always need to use the medications together. Agents associated with weight loss, like naltrexone, bupropion, phentermine, and metformin, can be used off-label for weight loss, alone or in other combinations (eg, bupropion with phentermine). HCPs should adjust as needed after determining what patients need. Do they have behavioral eating concerns? Are they snacking late at night? Are they experiencing binge eating? Do they have a preoccupation or intrusive thoughts related to food? Do they have another condition like depression where one of the agents can be used to treat the condition and support weight loss? The treatment should lean in to address the identified problem. It is important, however, to monitor patients when agents are used off-label.
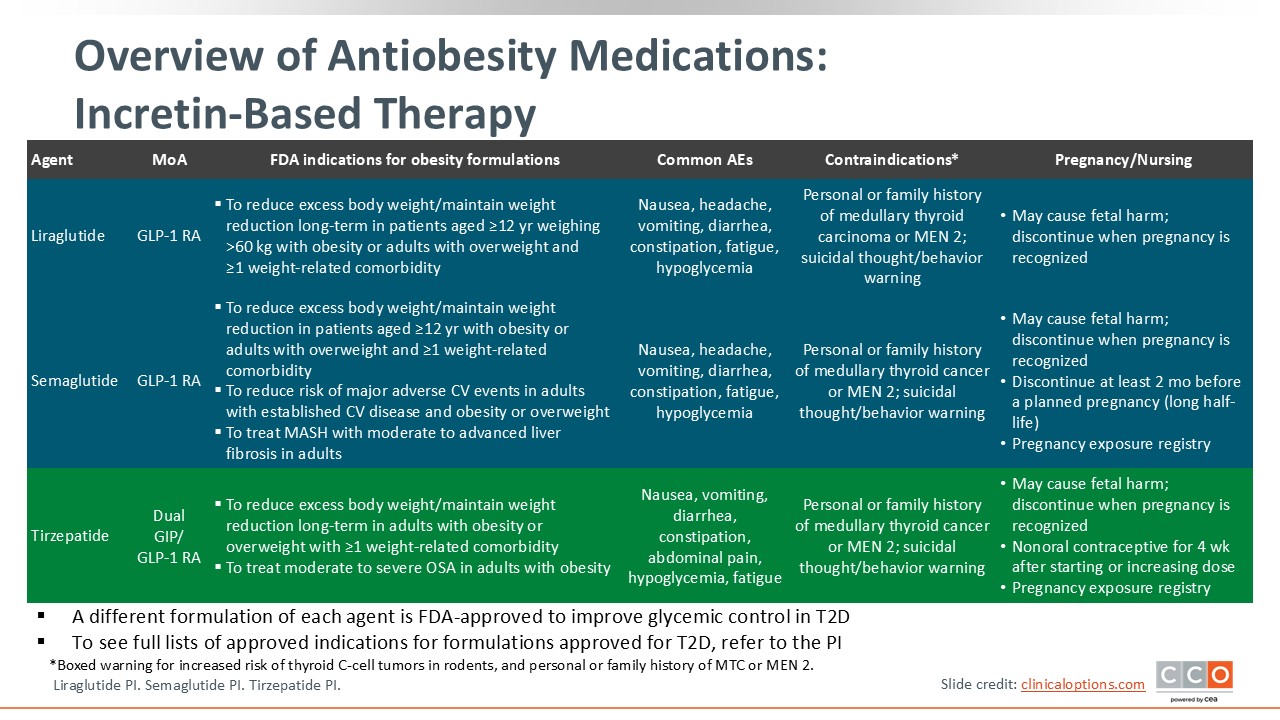
Overview of Antiobesity Medications: Incretin-Based Therapy
The incretin-based therapies include liraglutide, semaglutide, and tirzepatide, as well as other agents in development. These are not going to go away, and OB/GYN HCPs need to know about them because they can change patients’ lives. These agents are going to make a big difference in healthcare. They not only drive substantial weight loss but improve insulin resistance, cardiometabolic health, and fertility-related conditions like PCOS.
A critical point, however, is that incretin-based therapies should not be used during pregnancy.26-28 So HCPs should counsel patients on proper contraception and preconception planning.
Discussions on preconception planning and annual exams provide opportunities to make patients aware of the help OB/GYN HCPs can provide and to ask about future plans and goals.
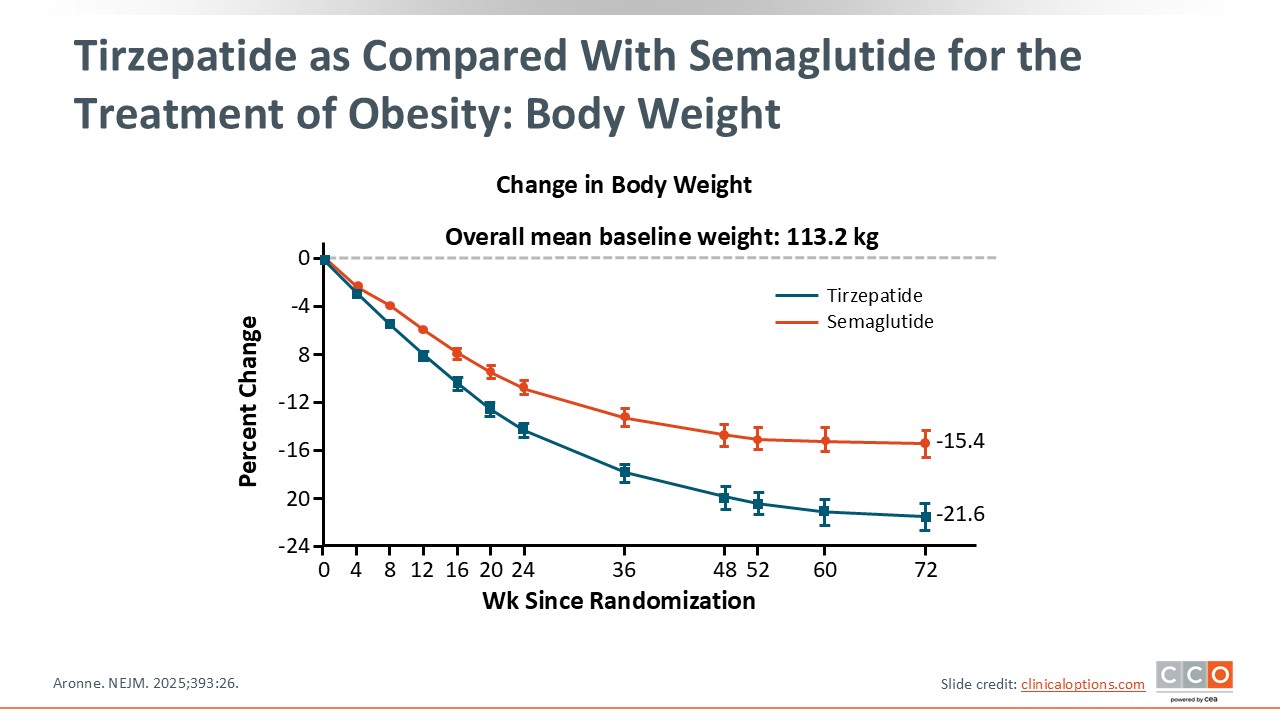
Tirzepatide as Compared With Semaglutide for the Treatment of Obesity: Body Weight
This figure presents information on 2 incretin-based weight loss medications that each yield substantial weight loss. Tirzepatide and semaglutide are both indicated to reduce excess body weight and maintain weight loss for adults with obesity or overweight and at least 1 weight-related comorbidity.27,28 The key takeaway from this is that both deliver substantial and sustained weight loss that exceeds previously available agents.
By 72 weeks, patients taking semaglutide lost 15.4% of their body weight, and those taking tirzepatide lost 21.6% of their body weight.18 Rather than focusing on one vs the other, the takeaway here is that the ingredients in these agents have transformed obesity care and hopefully will continue to do so for women's health. These agents produce double-digit, durable weight loss that previously was only achievable with metabolic/bariatric surgery. This means a lot to patients, but we must continue to select the right AOM based on their individual needs, comorbidities, access, and reproductive planning.
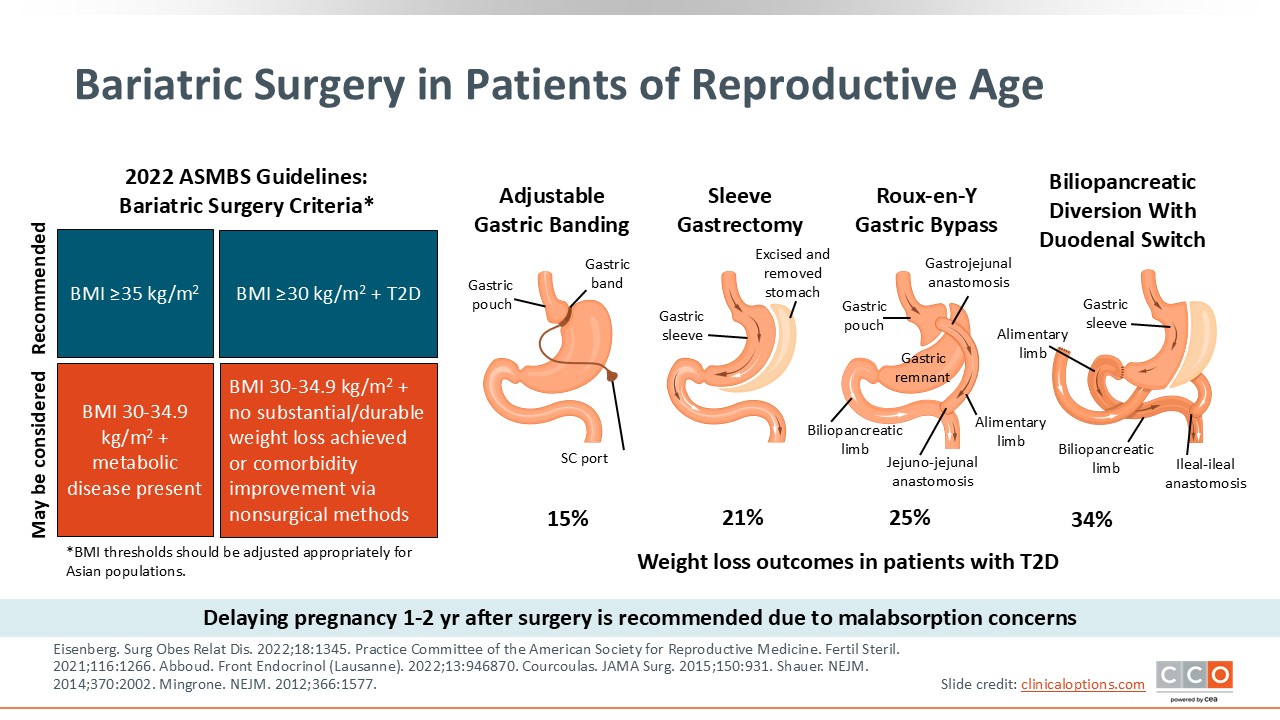
Metabolic/Bariatric Surgery in Patients of Reproductive Age
Talking more specifically about metabolic/bariatric surgery, this is a highly effective weight loss strategy. The data on this slide reflect weight loss for people with T2D, with approximate average weight loss ranges from 15% with gastric banding to 25% to 35% with bypass or duodenal switch surgery in these patients.29,30 Evidence indicates that people without T2D generally experience greater weight loss (approximately 5% more) than people with T2D.31 For your patients of reproductive age, the biggest thing to think about is timing. Patients should delay pregnancy for 1-2 years after surgery to achieve weight stability and address any malabsorption concerns.32
It is important to remember that OB/GYN HCPs should not actively encourage weight loss during pregnancy but should focus on promoting nutritional change. After metabolic/bariatric surgery, it is best to have weight stability before becoming pregnant.
The 5A’s of Shared Decision-making
How can OB/GYN HCPs offer obesity care with an already full schedule and without creating stigma and bias? The 5A's of shared decision-making can help by providing a framework for respectful and collaborative care.
First, “Ask.” Ask permission before doing an exam and addressing any sensitive topics. Asking permission sets the tone and avoids stigma.
Next, “Assess.” What are the patient's values, goals, and health risks? This goes beyond BMI. Do patients have comorbid diabetes? Are they at increased cardiovascular risk?
Then, “Advise.” Patients may come in and say they want to have a baby right away. Avoid blanket statements about avoiding pregnancy based solely on BMI. Instead, optimize health risks and create a plan with the patient.
This segues nicely into, “Agree.” HCPs should agree with patients on setting realistic goals and health outcomes together. Is it a realistic goal when a patient with a BMI of 50 kg/m2 presents to an OB/GYN HCP and says, "I want to lose 150 pounds before I have a baby in 6 months"? OB/GYN HCPs must work with patients to outline goals and expectations that all agree on.
Finally, “Assist.” This may mean helping patients identify and overcome barriers to care and/or treatment access, providing resources, and connecting them to support or referrals.33 Accessing AOMs, dietary/nutritional counseling, behavioral health, and even healthy food can often pose significant challenges for patients in OB/GYN care. OB/GYN HCPs see patients with these challenges daily, and it is vital that they partner with patients to provide comprehensive, personalized care.