CE / CME
Improving AATD Care Through Early Diagnosis and Multidisciplinary Management: A Call to Action
Physician Assistants/Physician Associates: 1.00 AAPA Category 1 CME credit
Nurse Practitioners/Nurses: 1.00 Nursing contact hour
Physicians: maximum of 1.00 AMA PRA Category 1 Credit™
Released: June 12, 2025
Expiration: June 11, 2026
Activity
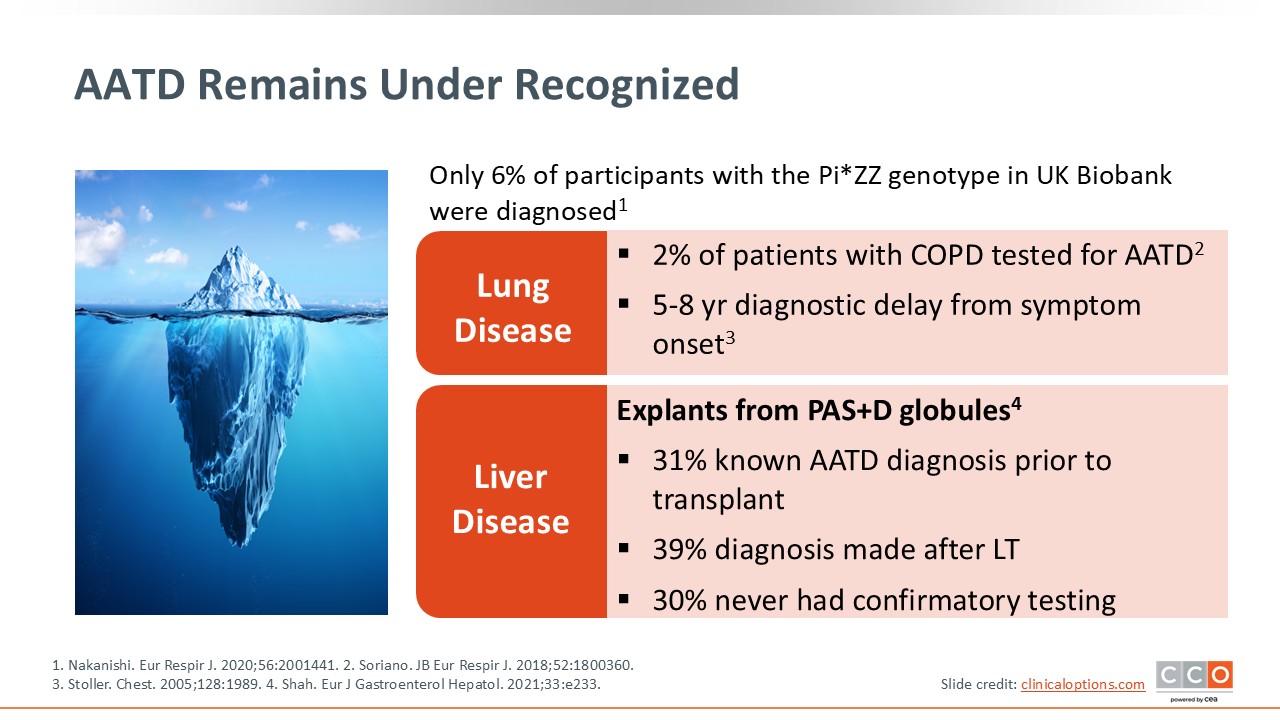
AATD Remains Under Recognized
AATD remains underdiagnosed. A study found that only 6% of participants with Pi*ZZ genotyping were diagnosed in the UK biobank. In addition, only 2% of patients with COPD are tested for AATD-related lung disease, and there is an average 5- to 8-year diagnostic delay from symptom onset to diagnosis.
In explants for PAS+D globules, 31% have a known AATD diagnosis prior to transplant, 39% have a diagnosis made after liver transplant, and 30% never have confirmatory testing.19-22
Why Is Early Diagnosis Important?
Diagnosing AATD early is important for improved survival and clinical outcomes, especially among never-smokers. There is increased incidence of liver cancer in individuals with AATD, although augmentation therapy for lung disease prevents additional loss of lung tissue. HCPs should implement preventive measures for patients, such as smoking cessation or avoidance, occupational counseling, avoiding alcohol, and maintaining healthy body weight with increased exercise.23-26
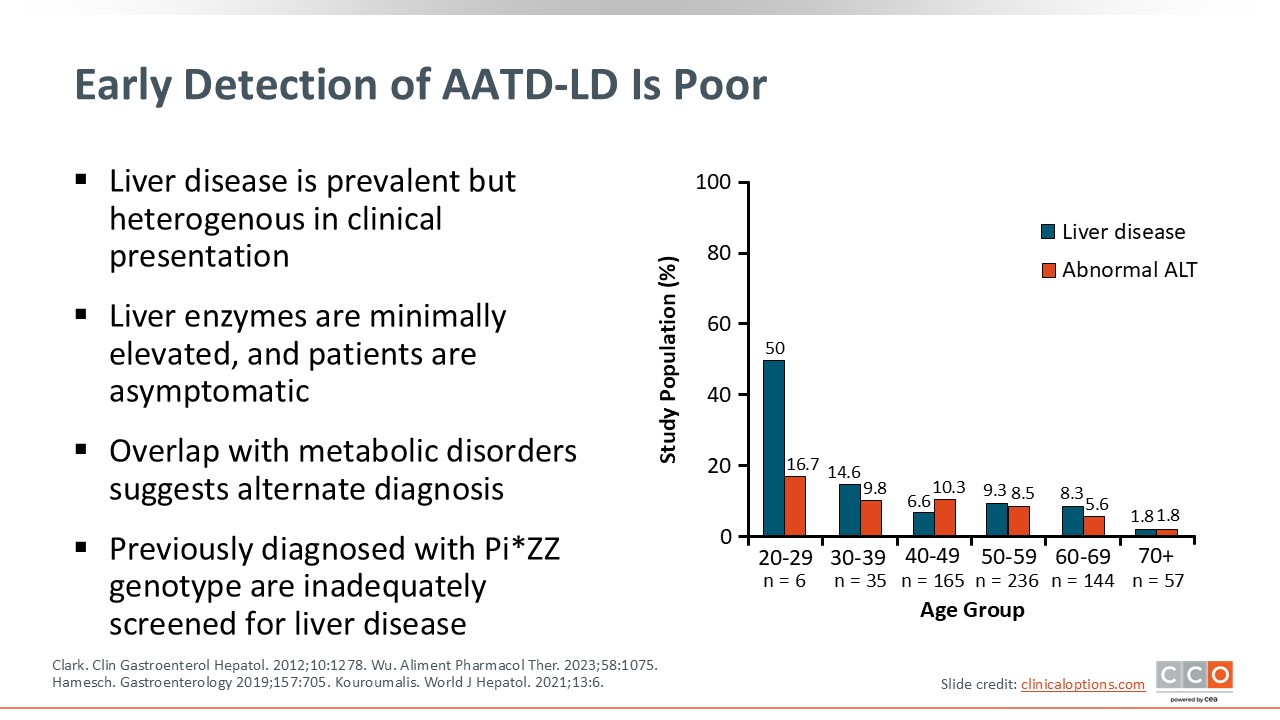
Early Detection of AATD-LD Is Poor
Early detection of AATD-associated liver disease is poor. Liver disease is highly prevalent but heterogeneous in clinical presentation. Furthermore, patients’ liver enzymes are often minimally elevated, and patients are largely asymptomatic.
There is overlap with metabolic disorders, which suggests alternate diagnoses. Patients may be diagnosed with fatty liver or other etiologies for elevated AAT and other liver enzymes. Unless patients with AATD and low levels of AAT are tested to determine genotype, they will remain undiagnosed. In addition, previously diagnosed patients with the Pi*ZZ genotype are inadequately screened for liver disease. Patients with AATD-related lung disease also are not adequately screened for fibrotic disease in the liver, which is important.27-30
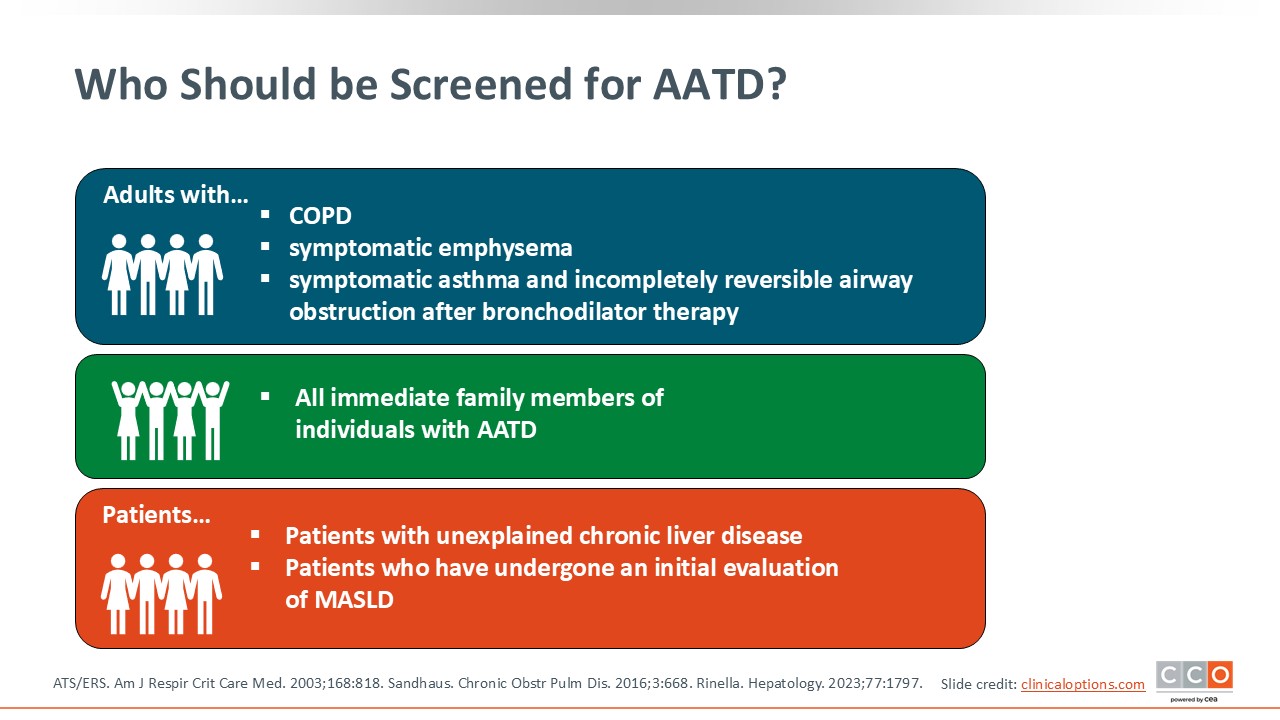
Who Should be Screened for AATD?
Adults with COPD, symptomatic emphysema, or symptomatic asthma with incompletely reversible airway obstruction after bronchodilator therapy should be screened for AATD. Furthermore, all immediate family members of individuals with AATD and patients with unexplained chronic liver disease or who have undergone initial evaluation for metabolic disfunction–associated steatotic liver disease should be screened for ATTD.31-33 Patients with elevated alanine transaminase or AST levels may be considered for testing AAT serum levels, followed by genotype or phenotype testing; whatever is available.
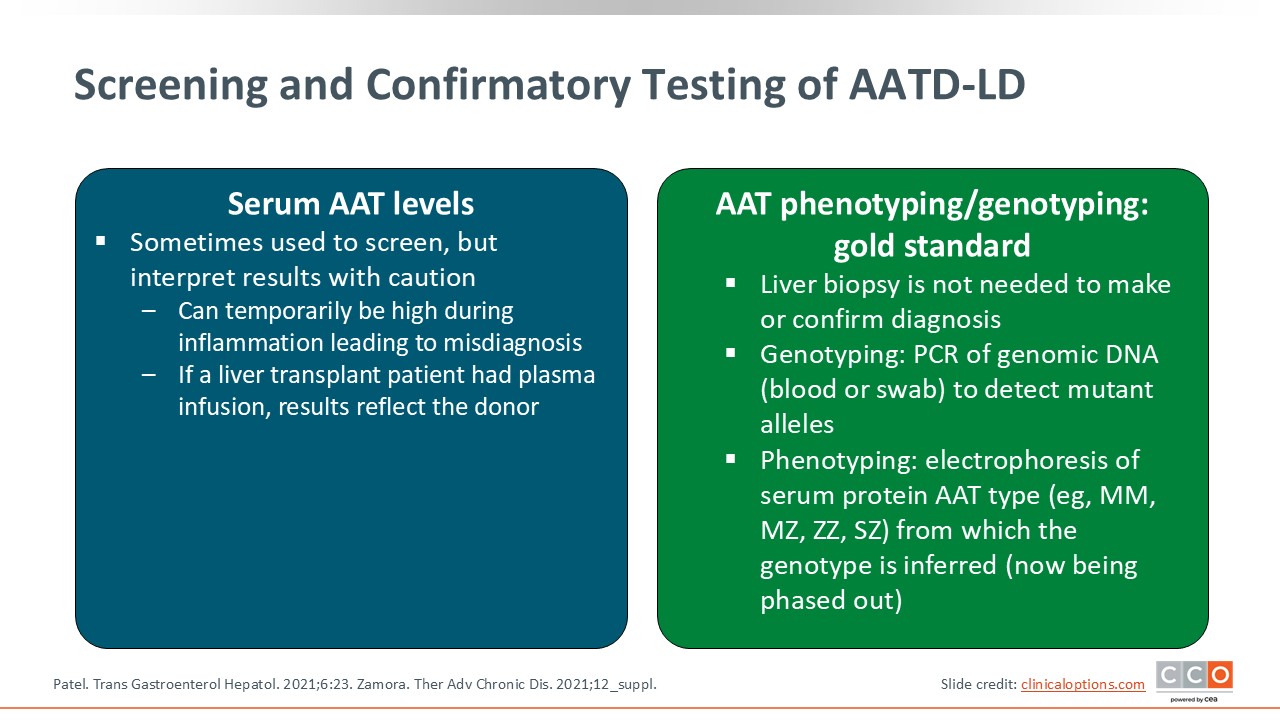
Screening and Confirmatory Testing of AATD-LD
Serum AAT levels are sometimes used to screen patients, but HCPs should interpret results with caution. These levels can be temporarily high during inflammation, and a transplanted liver will have plasma infusion results that reflect the donor, which leads to misdiagnosis. Rather, AATD phenotyping and genotyping are the gold standard. A liver biopsy is not needed to make or confirm a diagnosis. Genotyping can be done by polymerase chain reaction of genomic DNA via blood or swab to detect mutant alleles, and phenotyping can be done using electrophoresis of serum protein AAT type (eg, MM, MZ, ZZ, SZ) from which the genotype is inferred.1,34
Diagnosis of AATD
To diagnosis AATD, HCPs should measure patients' AAT and C-reactive protein (CRP) levels in serum and confirm with genotyping.9
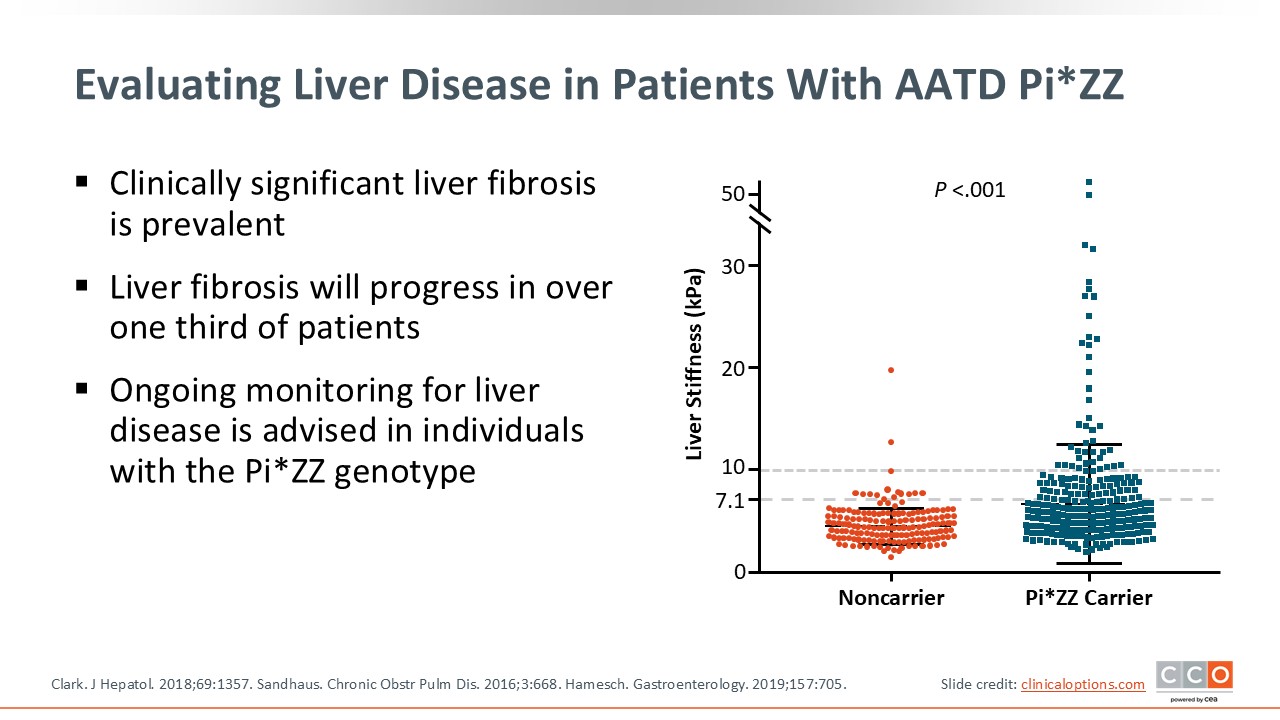
Evaluating Liver Disease in Patients With AATD Pi*ZZ
Clinically significant liver fibrosis is prevalent in those with AATD. It is typical to see a liver stiffness of 7.1 kilopascals (kPa) or higher via FibroScan associated with increased risk of fibrosis or fibrotic disease. These patients must be followed in the liver clinic. Liver fibrosis will progress in more than a third of patients. Therefore ongoing monitoring for liver disease is advised in individuals with the Pi*ZZ genotype.29,32,35
Click below to listen to Dr. Loomba’s comments about this topic.
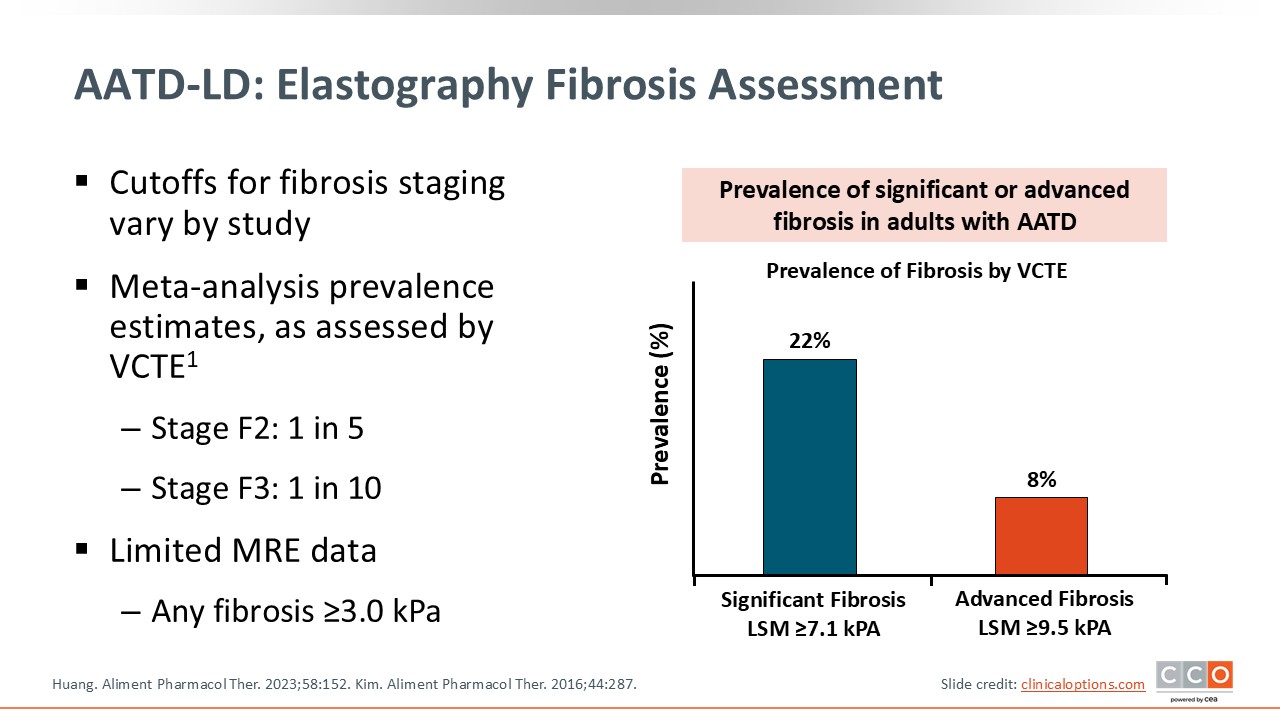
AATD-LD: Elastography Fibrosis Assessment
Significant fibrosis occurs in 22% of adults with AATD, whereas advanced fibrosis occurs in 8% of adults with AATD. Based on magnetic resonance elastography (MRE), any fibrosis of 3 kPa or higher is associated with fibrotic disease in AATD-related liver disease.36,37
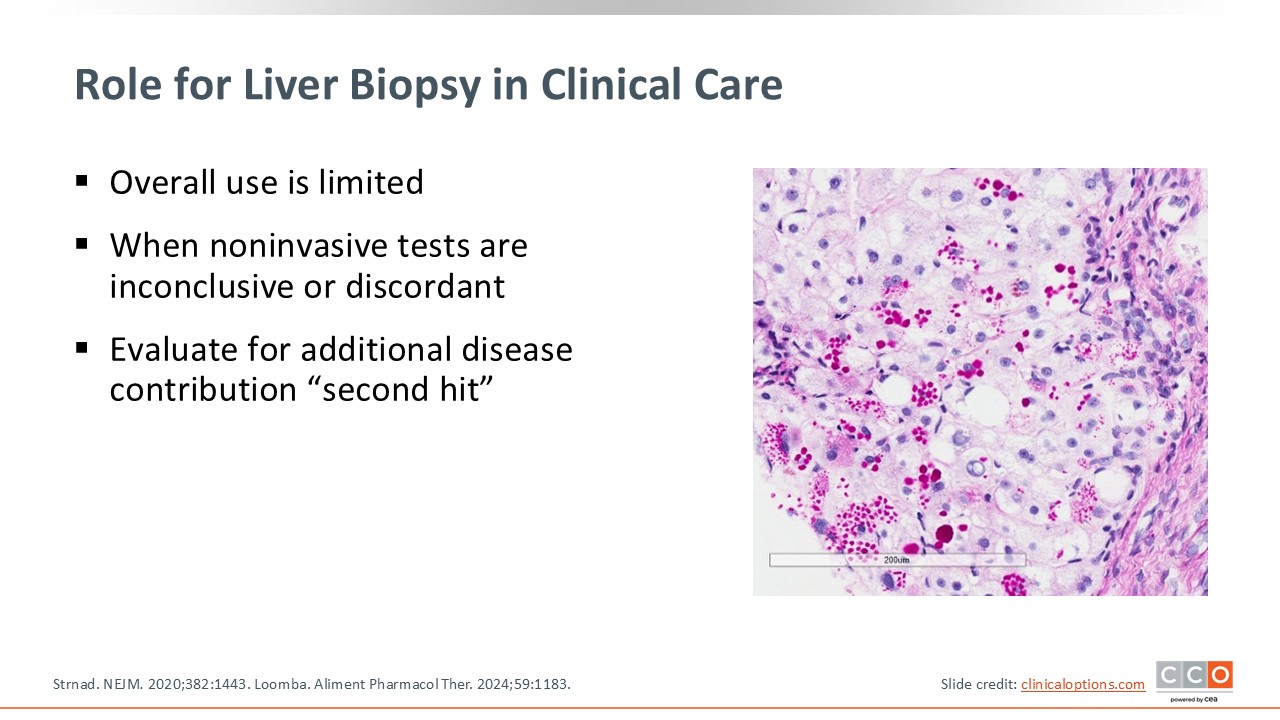
Role for Liver Biopsy in Clinical Care
Overall use of liver biopsy is limited. However, HCPs should consider liver biopsy assessment in patients where there is concern for a differential diagnosis or there may be a competing cause of their liver problems. When noninvasive testing is inconclusive or discordant, HCPs also should consider liver biopsy to evaluate for additional diseases that may be contributing as secondary factors.9,38
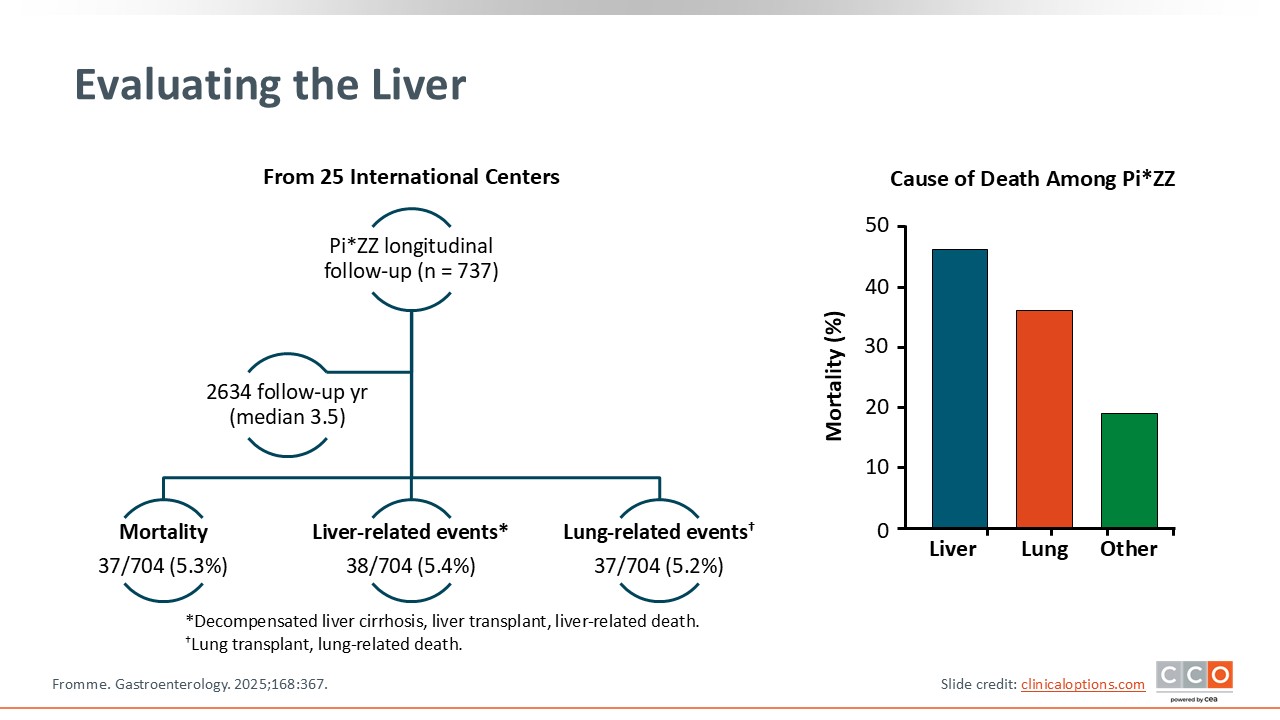
Evaluating the Liver
In evaluating the causes of death among patients with Pi*ZZ, the number 1 cause of death is liver disease, followed by lung disease, and other causes. This is why we must identify the patients who suffer from liver disease with the Pi*ZZ genotype. A longitudinal study of 25 international centers, 737 patients with Pi*ZZ and a median follow-up of approximately 3.5 years found a mortality risk of 5.3%, liver-related events risk of 5.4%, and lung-related events risk of 5.2%. Therefore, both liver-related morbidity and mortality and lung-related morbidity and mortality are important. We need to screen these patients for both lung and liver disease.39
Comparing Lung and Liver
This slide shows cumulative risk of liver disease and liver-related endpoints that are based upon liver stiffness; the higher the liver stiffness, the greater the risk of liver-related endpoints. When the FEV1 is low, the greater the risk of lung-related events.
Pi*ZZ patients with mild to moderate pulmonary function impairment or increases in liver stiffness have a 3 times higher risk of liver disease vs lung-related endpoints.39 Liver-related endpoints are important, and HCPs should identify these patients by doing liver stiffness assessment via FibroScan or MRE.
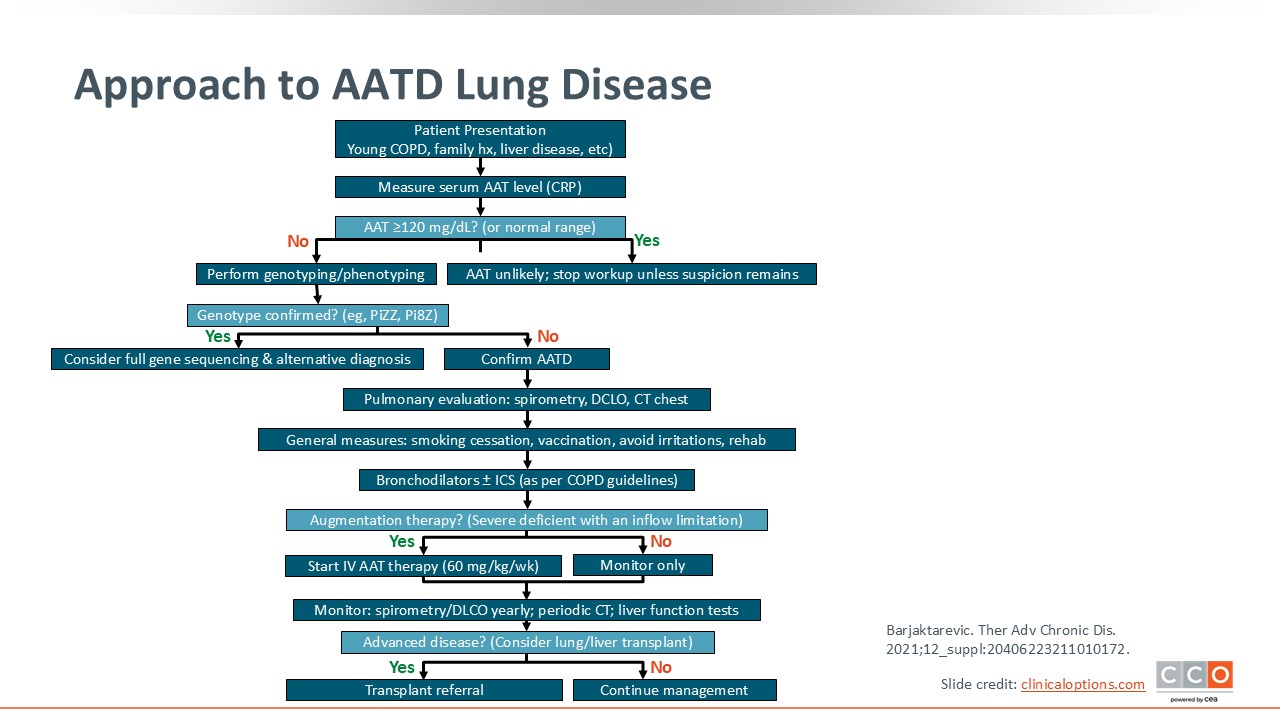
Approach to AATD Lung Disease
HCPs should test for AATD in patients with COPD regardless of age, family history of AATD, or unexplained chronic liver disease. HCPs can measure the serum AAT level or may consider CRP. If the AAT level is greater than 120 mg/dL or in the normal range, then AATD is unlikely. No additional workup is needed unless a suspicion remains.
If AAT levels are below 110 mg/dL, especially if below 100 mg/dL, then HCPs should perform genotyping. If the genotyping is confirmed as Pi*ZZ or Pi*SZ, then consider full gene sequencing or an alternate diagnosis. For those with confirmed Pi*ZZ, the AATD diagnosis also should be confirmed.
After which HCPs should consider pulmonary evaluation, as it is recommended in the guidelines. You can refer to a pulmonologist for patients to undergo spirometry, lung diffusion testing, and chest CT per the pulmonologist's expertise and evaluation.
General nonpharmacological measures for AATD-related lung disease include smoking cessation, irritant avoidance, and consideration of specific vaccinations. Pulmonary rehabilitation, particularly for those with already reduced lung function, is an effective approach for treating COPD, and its benefits are likely applicable to patients with AATD. Furthermore, pharmacological approaches, including bronchodilators and inhaled corticosteroids, may be used per COPD guidelines. Augmentation therapy should be considered in select patients, such as those with severe AATD and lung disease. Those with advanced disease may be referred for transplant. Patients who do not have compromised lung function should be monitored via annual spirometry or lung diffusion testing.14,32
I also recommend periodic liver function testing in these patients. Those with AATD-related lung disease and the ZZ genotype should be tested for liver disease using FibroScan, Fibrosis-4 index (Fib-4), or other biomarkers/serum levels like ALT, AST, and platelets).
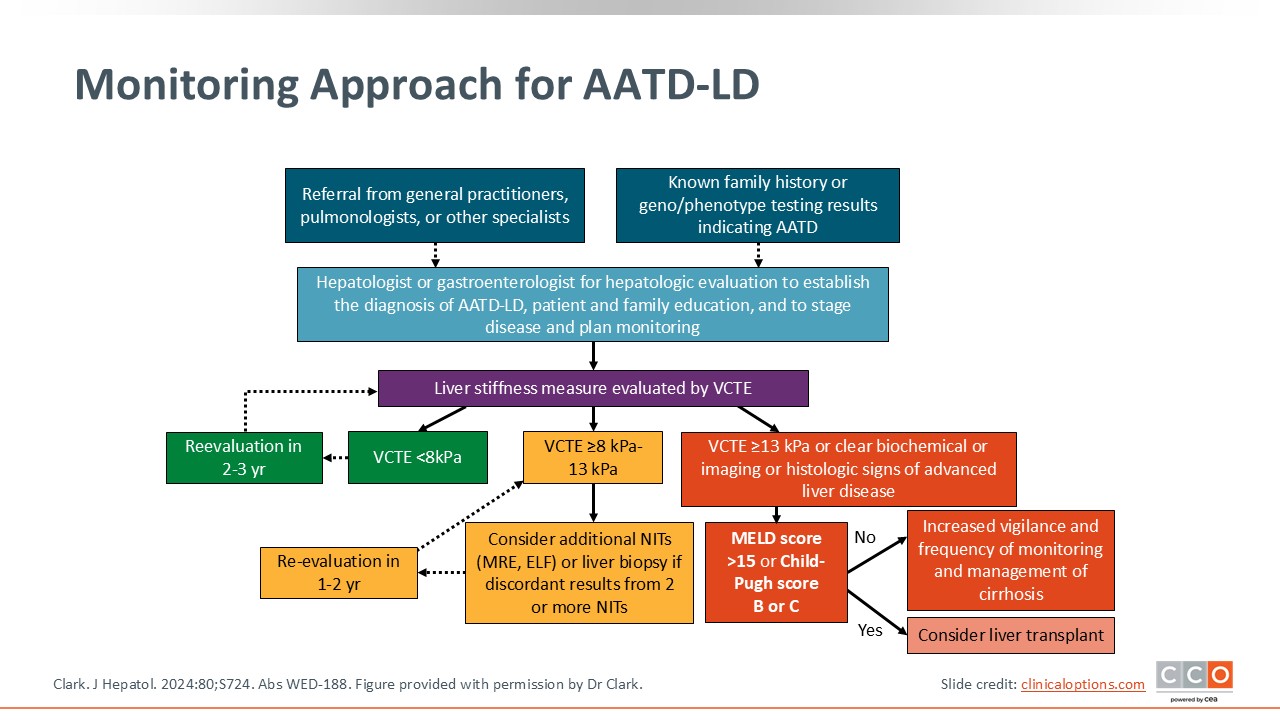
Monitoring Approach for AATD-LD
When addressing AATD-related liver disease, primary care providers, pulmonologists, and other specialists, should refer patients for assessment. All patients with a family history of or genotyping consistent with AATD should also receive liver assessment. Hepatologists or gastroenterologists should establish the diagnosis, stage, and monitor AATD-related liver disease. Furthermore, these specialists can provide additional education to patients’ family members.
In terms of liver assessment, HCPs may consider doing a Fib-4. If the Fib-4 is >1, patients may have fibrotic disease. HCPs also may consider doing liver stiffness measurement via vibration-controlled transient elastography (VCTE). If liver stiffness is <8 kPa, patients may be re-evaluated every 2-3 years. If liver stiffness is between 8-13 kPa, patients may have an increased risk for fibrotic disease. Additional testing such as MRE or an enhanced liver fibrosis panel can be considered, or liver biopsy should be done if noninvasive tests are discordant.
A liver stiffness of ≥13 kPa, clear biochemical or imaging evidence, or histologic evidence can indicate advanced liver disease. In these cases, HCPs might consider additional assessment to ensure that patients do not have cirrhosis. If cirrhosis is confirmed, patients need to be assessed for HCC screening and monitoring. Increased vigilance, monitoring, and cirrhosis management is required. And if a model for end-stage liver disease score reaches ≥15 or a Child-Pugh score is B or C, patients can be referred for liver transplant.40